A Runners Guide to Understanding and Avoiding Plantar Fasciitis
By William D. Charschan I.C.C.S.P.
If you have had plantar fasciitis, you know the pain, the difficulties walking and if you are an avid runner, it can stop you from running altogether. Many medical specialists know the condition by name and many podiatrists will typically manage it with foot orthotics, injections, sound wave therapy and in the worst cases surgeries that often, do not solve the problem (but may alleviate the symptom until it again exacerbates). Physical therapists often will try to strengthen the lower leg muscles, massage them, and even use proprioceptive tape that also may give you short term relief but may not alleviate the condition and prevent it from reoccurring. Even chiropractors have a solution of manipulation, soft tissue work, and exercises which may even work better, but may not solve the problem.
To solve plantar fasciitis, you need to first understand what the condition is. If you read the classical literature or Wikipedia, it will tell you the following;
“Plantar fasciitis (also known as plantar fasciopathy or joggers heel) is a common painful disorder affecting the heel and underside of the foot. It is a disorder of the insertion site of ligament on the bone and is characterized by scarring, inflammation, or structural breakdown of the foot’s plantar fascia. It is often caused by overuse injury of the plantar fascia, increases in exercise, weight, or age. Though plantar fasciitis was originally thought to be an inflammatory process, newer studies have demonstrated structural changes more consistent with a degenerative process. As a result of this new observation, many in the academic community have stated the condition should be renamed plantar fasciosis.[1]“ Read more here.
While the classical ways most healthcare providers and even runners treat the condition rarely work long term, because of a fundamental misunderstanding of what plantar fasciitis is and why it developed. All too often, we treat the symptom of where it hurts (the feet), instead of why it hurts.
The typical plantar fasciitis patient is a heavy heel striker (not necessarily someone who is overweight), may have either very flat feet or high arches , or perhaps a combination of both and is often but not always inflexible. In this author’s experience, almost all are built asymmetrically, which causes their core muscles (muscles in the mid-section of your body) and the pelvis to distort.
, or perhaps a combination of both and is often but not always inflexible. In this author’s experience, almost all are built asymmetrically, which causes their core muscles (muscles in the mid-section of your body) and the pelvis to distort.
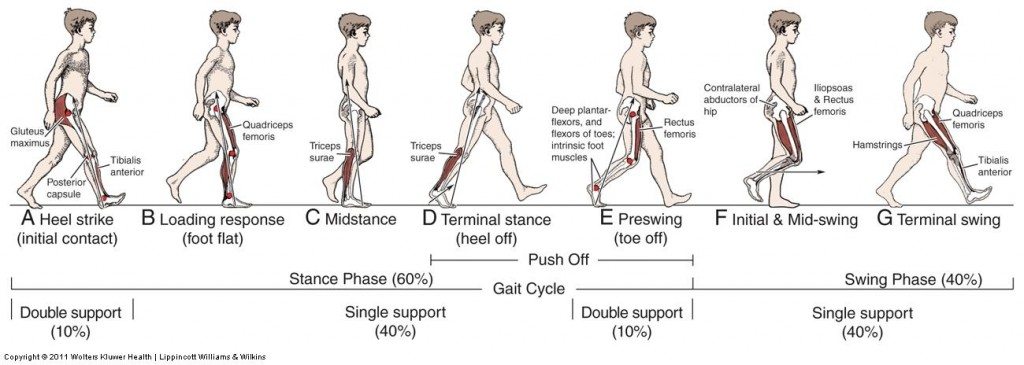
When this occurs, we lose the dissipation of shock that the pelvis provides, while the myofascia that surrounds the core will tighten in response to this now asymmetrical loading, resulting in a torqued or distorted core that is poorly trainable and will often result in back pain and even neck pain. When the core distorts, the legs will tighten over time as well, affecting the coordination of movement during the normal gait cycle (the way you walk), and decreasing the shock absorption from the heel through the pelvis.
Normal subtle movements of the leg such as pronation of the foot turn out a little as we toe-off (step off our toe), helps to absorb shock through the knee and the hip while we walk. Inherited body asymmetries affect this by causing a distortion of the pelvis, reducing the stability of our core and affecting the ability to absorb shock from the heel through the hip and pelvis, resulting in a harder impact on the body structures, especially the back of the legs and the calves which continue to tighten, affecting the plantar fascia, the heel, and the surrounding tissues.
To understand this concept further, the pelvis is responsible for at least 50 percent of the motion of the body and it is where the body derives power and leverage from in an X pattern as we walk and do other activities. If the core is distorted, we will over and under stride from side to side (one leg will take shorter steps while the other takes longer ones), with compensation of this occurring in the upper body, which causes poor absorption of impact from the ground up.
As mentioned previously, when you heel strike, your foot is supposed to pronate (turn out a little) which brings you into toe-off. At the point of impact, the ankle should absorb shock through the heel, foot and ankle bones, tibia, the gastroc, and the gluteal muscles as they act as a spring. A mechanism at the knee called the screw home mechanism rotates the knee a little internally (which also absorbs the shock) and those same forces are then absorbed and dissipated at the hip and pelvis.
As you can see, throughout a normal gait cycle, shock needs to be absorbed. We adopt to a more adult style gait from the time we are about 6 yrs. old as we grow and develop skeletally and muscularly. , If we are tight or stiff from a lack of spring which will affect the tightness of the surrounding fascia and the muscular tissues, we believe that it is normal or normal for us, since we have no experience feeling anything else. The truth is, there is no well-defined normal, although a range of normal sort of exists in medical circles, however, there is a perception that a lack of pain is normal and pain is abnormal. This concept is explained in detail in the book Cheating Mother Nature, what you need to know to beat chronic pain. The book is a great read for anyone who wants to understand why they hurt.
Most healthcare visits are about your symptoms, where the symptoms are and treating the area of complaint, however, unless the functional reason for plantar fasciitis is addressed (lack of spring and repeatedly high impact) the condition will reoccur, or stress fractures may develop. Looking at the foot or the heel, without understanding or resolving the mechanism behind the condition cannot possibly be good for your running, your comfort, or the joints in your foot, ankle, knee, and hip.
A better approach to the problem
You cannot place your profession first and use it as a lens to fix a problem such as plantar fasciitis. This is known as physician bias and is most likely why most people with this condition never fully resolve or have the condition return. Cushioning, or foot orthotics alone is not enough to resolve the problem, but it may relieve the pain somewhat. Your healthcare practitioner must look at your body mechanics, how you walk, your body symmetry and style of gait, and understand how you hit the ground. Your healthcare practitioner must evaluate the springiness in your feet and the fascio kinetic chain (series of joints from your ankle to your hip) which can be done during a full biomechanical evaluation, which looks at passive leg movements such as flexion, internal and external rotation and understands if there are any restrictions to the normal spring mechanisms of gait on both feet.
Care must be given to restore normal shock absorption at the calf, knee, hip, and pelvis, and the secondary compensations in the upper body must also be resolved to successfully resolve the condition.
Often the most effective way to treat and resolve involves myofascial release treatment, other soft tissue methods such as the Graston Technique which uses instruments and is superior in its ability to loosen fibrotic tissue restricting movement and manipulation of the extremities and pelvis which is most commonly done by chiropractors. After treatment, your doctor should retest to see if the springy end feel has returned to the joints in the foot and leg and to check to see if the firing patterns in the leg have improved (the coordination of movement) which will markedly decrease the likelihood of a reoccurrence.
While the medical establishment is trying to treat the condition, running shoe manufacturers already understand that if you decrease impact, the person feels better. Newer running shoes are being released that are maximalist (vs. minimalist, the recent craze that has come and gone) and shock-absorbing shoes are now popular.
While these shoes may not solve all your mechanical problems, they seem to control the foot more with a straighter last (a style of shoe sole ideal for overpronators) and a way of absorbing ground shock and enhancing your body mechanics as you walk or run in the shoes.
While barefoot runners believe that only a barefoot running style will properly absorb shock from their feet, they too have problems mechanically and end up with foot pain and running injuries, so shoes or not, the way your body functions at impact will cause the condition.
You cannot change your running style away from tight myofascia, a poorly working gait cycle, and a compromised core. These problems need to be fully addressed to get a great result with plantar fasciitis.
What to do to get out of pain
- A proper musculoskeletal evaluation using active evaluation methods. This assures that the likelihood of an appropriate diagnosis which will lead to an effective treatment regimen.
- Fascial manipulation using Myofascial Release (active release techniques is a style of this), instrument assisted soft tissue methods such as Graston.
- Manipulation of the extremities, pelvis, and spine to assure proper joint play and alignment, usually done by chiropractors. Movement and symmetry are the key to a properly functioning core and a better, less impactful running gait.
- Active rehabilitation regimens with corrective exercises to retrain the gait cycle.
- Hip socket stretching protocols if the joints themselves have tight hip capsules. This a common compensation is seen in many plantar fasciitis sufferers often ignored by most healthcare practitioners who were never trained to evaluate and properly treat it.
- A post-treatment treadmill analysis to evaluate gait asymmetries post-treatment and to evaluate the intensity of impact at the ground. Treadmills are a great way to evaluate yourself. To properly do a treadmill evaluation, get on the treadmill at a comfortable running speed, increase the speed a little past your comfort zone, and shoot a 30-second video from the side and the back. You may be surprised at what you will find.
Read Cheating Mother Nature, what you need to know to beat chronic pain available through Amazon.com